A Comprehensive Guide to Electrophysical Agents (EPAs)
By: Estimated reading time: 18 minutes
By: Estimated reading time: 18 minutes
Introduction
There are many kinds of Electrophysical Agents (EPAs) that rehabilitation practitioners may use. You may remember racking your brain while learning about EPAs in school, trying to understand how they work, how to use them, and the contraindications to their use. In this blog, we will provide you with a basic overview of common EPAs, including what they are, what they are used for, as well as their parameters and contraindications. There is a chart included at the end of this blog with a summary of parameters for common EPAs.
It is important to note that there is limited evidence supporting the use of EPAs and variation in recommended parameters. Therefore, it is imperative that clinicians use their clinical reasoning alongside available evidence and practice guidelines in order to make the best decisions and recommendations for each of their patients. Additionally, with many EPAs, there is a risk of tissue damage if not used appropriately. Remember to conduct frequent skin checks and ask your patient to report if they feel discomfort. Do not apply EPAs to a patient that has sensory or cognitive impairments that will make it difficult for them to feel or communicate if they are experiencing discomfort.
Thermal Agents
Heat:
What is it?
Heat agents refer to modalities that heat the skin and superficial tissues within 1-2mm. Some examples are a hot pack, whirlpool bath, hot wax, contrast baths, and fluidotherapy.
What is it used for?
Heat modalities are used to relieve pain by stimulating A-delta and C nerve fibres which inhibit pain transmission at the dorsal horn of the spinal column. Heat modalities also cause vasodilation, enhance tissue repair, increase tissue extensibility, and decrease muscle tone and spasms. Based on this, heat modalities can promote tissue healing and therapeutic movement, however, should not be used during the acute inflammatory stage of healing.
Parameters:
For a therapeutic effect, aim to heat tissues to approximately 45 degrees celsius. Specific parameters to reach this temperature will depend on the kind of heating modality that you are using.
Contraindications:
Do not apply heat modalities to large areas resulting in increased core temperature in patients who are pregnant or have cardiac disease. Do not apply over malignancy, recently radiated tissues, infection, bleeding tissues, area of impaired circulation, inflamed tissues, heat-sensitive skin disease e.g. eczema, severe edema, or reproductive organs. Do not utilize heat modalities for patients with hemorrhagic disorder, deep vein thrombosis, impaired sensation or cognition.
Cold:
What is it?
Cold agents are modalities that cool superficial tissues, and deeper tissues if applied for a long enough period of time. Examples include ice packs (this warms up quickly and therefore are not recommended), crushed ice, ice water bath, coolant spray, quick ice, cool whirlpool and contrast baths.
What is it used for?
Cold modalities are used for the treatment of acute injury to reduce pain, cause vasoconstriction which prevents inflammation, stop bleeding, reduce muscle spasms, and reduce the risk of secondary injury to tissues due to hypoxia after injury by slowing down tissue metabolism.
Parameters:
When using crushed ice, apply over a damp towel, not directly on the skin, for 10 minutes to modulate pain, or for 18 - 20 minutes to cool deep tissue and prevent inflammation. For other cold modalities, refer to their manuals for instructions.
Contraindications:
Do not apply cold modalities to a person with a cold allergy, Raynaud’s disease, cryoglobulinemia or hemoglobinemia. Do not apply over an area of impaired circulation, chronic wounds, regenerating nerves, tissues impacted by tuberculosis, anterior neck and carotid sinus. Do not apply cold modalities to a person with a hemorrhagic disorder, deep vein thrombosis or impaired sensation and cognition.
Ultrasound
What is it?
Ultrasound therapy is the delivery of high-frequency mechanical energy to tissues via vibration of a transducer, either with thermal or non-thermal effects depending on the parameters used.
What is it used for?
Ultrasound affects tissues at the cellular level resulting in an accelerated inflammatory process and a good environment for tissue repair. Thermal ultrasound has the additional effect of heating tissues, resulting in the effects described above for heating modalities (i.e. vasodilation, enhanced tissue repair, increased tissue extensibility and decreased muscle tone and spasms), but should not be applied during the acute inflammatory stage of healing. Athermal ultrasound may be applied during the acute stage.
Parameters:
Ultrasound should be applied on a continuous setting to produce thermal effects, and on a pulsed setting for non-thermal effects.
For continuous ultrasound, intensity should be set between 0.8-2 W/cm SATP, but only as high as is necessary for the patient to feel some heat, and should be applied for 10-15 minutes per 10cm.
Pulsed ultrasound means that it is on for a percentage or ratio of the time, known as the duty cycle. Pulsed ultrasound should be set at a duty cycle of 20% aka 1:4 on-off ratio and at an intensity of 0.1-0.2 W/cm SATA (ie. average intensity) or 0.5-1 W/cm SATP (i.e. peak intensity). (Tip: SATA is 20% of SATP because we use a 20% duty cycle.) Pulsed ultrasound should be applied for 10-15 minutes per 10-15 cm. For either continuous or pulsed ultrasound, set the frequency to 3 Hz to treat superficial tissues, or 1 Hz to treat deeper tissues (3-5 cm depth). Apply ultrasound gel to the skin and then move the ultrasound head over the tissue that you wish to treat at a speed of 2-4 cm/s. Ensure the ultrasound head is flat on the tissue surface.
Contraindications:
Do not apply ultrasound therapy over the eyes, abdomen during pregnancy, testes, malignancy, vascular insufficiency, heart, acute infection/sepsis or bleeding tissues. Additionally, do not apply thermal ultrasound if the patient lacks sensation or may have difficulty communicating if they feel discomfort. Be cautious of applying ultrasound over implanted electronic devices and metal and plastic implants.
Electrical Stimulation
Transcutaneous Electrical Nerve Stimulation (TENS)
What is it?
TENS is the use of relatively low-frequency, pulsed electrical currents applied to the skin via electrodes.
What is it used for?
TENS is used to temporarily relieve pain. Conventional TENS (C-TENS) depolarizes A-beta nerve fibres which leads to reduced nociceptive inputs to the spinal cord, modulating the ascending sensory pathway. Acupuncture-like TENS (A-TENS) depolarizes A-delta and C fibres which activates the descending sensory pathways and results in the release of endogenous opioids. Both methods result in reduced pain experience, however C-TENS is typically trialled first as it is less intense. It is possible that A-TENS has longer-lasting effects than C-TENS, however this is debated in the literature. TENS units can be relatively inexpensive making them more accessible to patients who wish to self-administer TENS at home to relieve pain.
Parameters:
C-TENS is described as “low intensity / high frequency” since amplitude (intensity) should only be raised until the patient feels a sub-noxious tingling sensation, and frequency is set between 80-120 Hz. Pulse duration should be set at 150-200 microseconds (µs). Pain relief from C-TENS occurs mainly while it is being used, lasting maximum 20 minutes afterwards, but it can be applied as long as the patient wants (with skin checks every so often). Electrodes should be placed over the area of pain, bracketing the pain, over the dermatome, or over muscles at the corresponding spinal level.
A-TENS is described as “high intensity / low frequency” since amplitude should be gradually increased to quite a high point at which non-painful muscle twitching occurs, but the frequency is set low between 3-10 Hz. Pulse duration should be set at 250 µs. A-TENS should be administered for 15-30 minutes and may be repeated after 4 hours, as needed, but it should not be administered as frequently as C-TENS. Electrodes should be placed over the dermatome, trigger points or acupuncture points.
Contraindications:
Do not apply TENS over electrically sensitive support systems, chest wall if the patient has a heart condition, autonomic plexus if the patient is hyper/hypotensive, abdomen/lumbar area if the patient is pregnant, carotid sinus, thrombosis, neoplastic tumour, infected tissue, hemorrhaging tissue, or if the patient has a history of seizures.
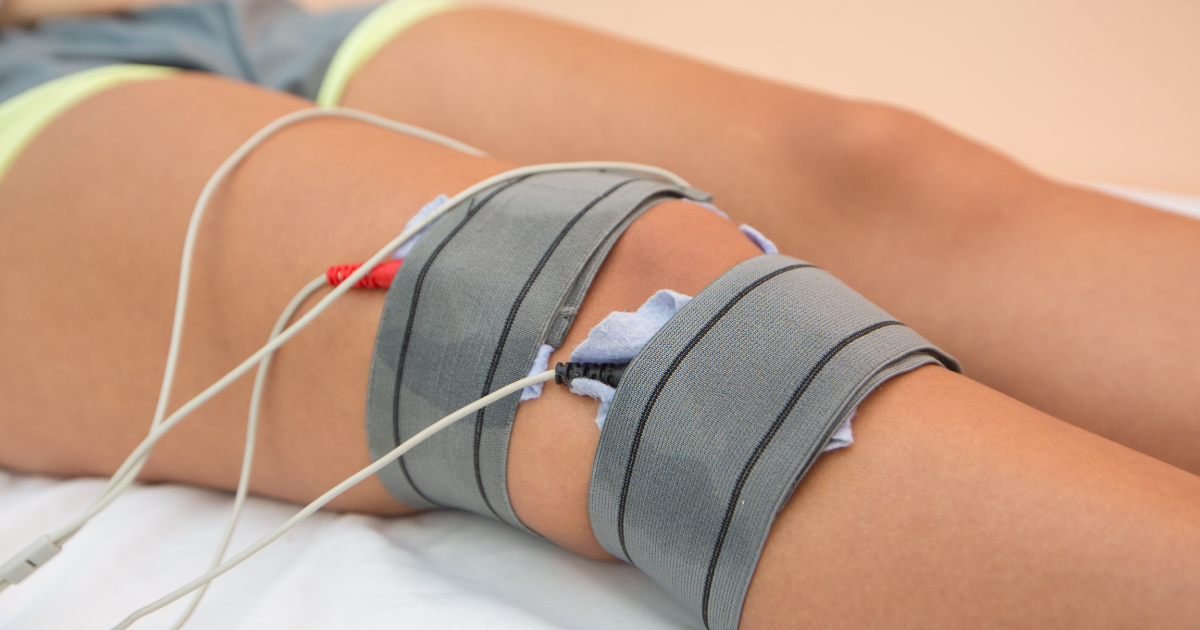
Interferential Current (IFC)
What is it?
IFC is similar to TENS in that it uses electrical currents to modulate pain. However, while TENS utilizes one relatively low-frequency current, IFC involves two medium-frequency currents (4 electrodes) that interfere with one another below the skin, creating a resultant low-frequency current within painful deep tissues in order to modulate pain.
“Why is the frequency of these modalities important?”, you may ask. It is important because
- Research indicates that low-frequency currents modulate pain.
- Skin impedance (resistance) is inversely correlated to a current's frequency. This means that there is high skin impedance to a low-frequency current, making low-frequency currents (e.g. TENS) uncomfortable and it difficult for the current to penetrate to deep tissues.
IFC uses medium frequency currents instead, which have lower skin impedance, making it a more comfortable modality, especially when treating deeper tissues or larger areas. The key is that IFC results in a low-frequency current within the tissue, and therefore it is able to modulate pain while being more comfortable. (This is the theory behind IFC, but it is debated somewhat in the literature.)
What is it used for?
IFC is used to temporarily relieve pain, especially in deeper tissues or large treatment areas.
Parameters:
IFC involves 2 currents. One is set at a carrier frequency of 4000 Hz, and the second current is set at a slightly higher frequency, known as the Amplitude Modulated Frequency (AMF). The parameters can be set for immediate pain relief or more intensely, for longer pain relief (similar to C-TENS vs A-TENS).
For acute pain relief, the carrier frequency should be set to 4000 Hz, and the AMF to 80-120 Hz (i.e. the frequency of the second current is 4080-4120 Hz). The second current can stay at one frequency or sweep within the range of frequencies, gradually increasing for six seconds and then gradually decreasing for six seconds.
For longer pain relief, the carrier frequency is also set to 4000 Hz, while the AMF is set lower at 1-10 Hz. The frequency sweep should occur abruptly so that the frequency of the second current is relatively high (i.e. 10 Hz) for 6 seconds and low for 6 seconds.
For both methods, apply the modality for 20-30 minutes. Self-adhesive pad electrodes, pad electrodes with sponges, or suction electrodes with sponges can be used and should be placed over the area of pain, bracketing the pain, over the dermatome, or over muscles at the corresponding spinal level. If using the suction electrodes, apply constant suction for acute pain relief, and intermittent suction for longer pain relief.
Contraindications:
Do not apply IFC with an ice pack, over an area of impaired sensation or if the patient may have difficulty understanding or communicating if they are experiencing discomfort. Do not use small electrodes as this may lead to tissue damage/burns. Do not apply IFC over electronic implants, the abdomen / lumbar areas if the patient is pregnant, deep vein thrombosis, hemorrhaging tissue, infection, damaged skin, anterior neck or area of malignancy within the past six months.

Neuromuscular Electrical Stimulation (NMES)
What is it?
NMES is the application of electrical currents via electrodes to stimulate intact lower motor neurons in order to activate paretic/paralyzed muscles.
What is it used for?
NMES can be used to strengthen specific muscles or to activate a group of muscles in a specific sequence to assist a patient in carrying out a functional task (e.g. grasping an object). This sub-type of NMES is known as functional electrical stimulation (FES). NMES can help manage spasticity, and act as neuroprosthesis (e.g. activating ankle dorsiflexors instead of using a traditional ankle-foot orthosis to address drop foot). Because of the above applications for NMES, it is commonly used in neuro rehab, when treating a patient after a stroke or spinal cord injury.
Parameters:
NMES utilizes a symmetrical biphasic waveform. At the beginning and end of each muscle activation cycle, there should be a ramp time of 1-2 seconds during which the current gradually turns on and off.
- To improve muscle strength (up to grade 3 MMT): The frequency of the current should be set at 50 Hz and pulse duration at 300 µs. There should be an “on” time of 10 seconds (including ramp up and down) when the muscle will contract and an “off” time of 50 seconds when the muscle will relax. When determining the amplitude, slowly increase the intensity until the muscle fully contracts and then set the machine at this amplitude. Have the patient do 10-15 repetitions of muscle contractions, or less if the muscle is fatigued earlier.
- To improve muscle endurance: Frequency should be set between 25-30 Hz (which is lower than strength training, to prevent early muscle fatigue) and pulse duration at 300 µs. There should be an “on” time of 10 seconds (including ramp time), and an “off” time of 12 seconds. This ratio can be progressed to 30 seconds on, 2 seconds off. Increase the intensity slowly until an amplitude causes the muscle to fully contract. Administer this treatment for 10-15 minutes, progressing to multiple hours per day. Stop when the muscle fatigues.
- To manage spasticity: Use a frequency of 35-50 Hz and pulse duration of 150-200 µs for small muscles or 200-350 µs for large muscles. On and off time should be the same length, between 2-5 seconds including ramp time. As above, increase the amplitude until a full contraction is elicited. Apply the electrical stimulation to a spastic muscle to fatigue it or to an antagonist muscle to cause reciprocal inhibition of the spastic muscle. The duration of treatment should be 10-30 minutes, every 2-3 hours until the spasticity is decreased.
For all of the above methods, place one electrode over the motor point (area of easiest excitability of a muscle) or nerve supply to the relevant muscle, and the other electrode distally.
For functional activities or for use as a neuroprosthesis, use an FES modality that is manufactured for that specific task, and review the instructions for applicable parameters.
One central principle about NMES that is important to remember:
The patient must actively try to engage the muscles when the modality is on, in order to promote optimal motor learning.
Contraindications:
Do not apply NMES over electrically sensitive support systems, carotid sinus, chest wall, major autonomic plexus in a patient that is hypo/hypertensive, thrombus, malignancy, infection, abdominal/lumbar/pelvic area of a pregnant patient, or over craniofacial/cervical areas if the patient has a seizure history. Do not apply NMES to a patient that lacks sensation or has cognitive impairments that may make it difficult for them to understand or communicate if they are experiencing discomfort. Do not use NMES within 10 meters of a shortwave diathermy device.
Iontophoresis
What is it?
Iontophoresis is the use of electrical current to promote the absorption of medications across the skin. Positively charged ions in cationic medications are repelled across the skin by the anode (negative electrode). Negatively charged ions in anionic medications are repelled across the skin by the cathode (positive electrode).
What is it used for?
Iontophoresis may be used to transdermally apply anesthetics, antibiotics, anti-inflammatories and various other medications that are prescribed by a physician when the use of an oral medication, topical cream or needle is not appropriate or possible (e.g. needle phobia, avascular tissue). It is also used to treat hyperhidrosis (excessive sweating) and to reduce hypertrophic scars.
Parameters:
Iontophoresis utilizes a Galvanic current (i.e. direct current, flows in one direction). The total dose is typically 40mA*min, which is the amplitude of current flowing, multiplied by time during which the current is flowing. However, in order to determine what amplitude to use, it is important to be aware of a concept called current density, which is the concentration of the current. Excessive current density may result in burns. A safe current density is between 0.1-0.3 mA/cm, though these numbers are debated in the literature. To calculate an appropriate amplitude, you may utilize the following equation:
Amplitude (mA) = safe current density (mA/cm) x electrode area (cm)
Next, calculate the treatment time required to deliver the total dose at the amplitude you have determined above.
Treatment time (minutes) = total dose (mA*min) / amplitude (mA)
When applying iontophoresis, place one electrode over the area of desired medication delivery, and the other electrode over a remote site. The remote electrode can be larger than the electrode over the treatment area, to disperse the current.
Contraindications:
Do not use iontophoresis over open skin, temporal/orbital regions, implants and anterior chest of cardiac patients. Do not use iontophoresis if the patient has skin allergies, an allergy to ions, impaired sensation or cognitive impairments that may make it difficult for them to understand or communicate if they are experiencing discomfort.
Light Amplification from Stimulated Emission of Radiation (LASER)
What is it?
Laser therapy is the use of a specific kind of light applied to the skin to treat pain and inflammation and promote tissue healing. Light from a laser is unique in that it is monochromatic (one colour, has a narrow bandwidth), collimated (light waves are all parallel and so the light does not spread) and coherent (light waves are the same frequency and in phase i.e. peaks and valleys coincide).
For therapeutic purposes, there are “cold” and “hot” types of lasers.
Cold lasers are known as low-level laser therapy and have a power of less than 0.5 W, while hot lasers are known as high power laser therapy and have a power of greater than 0.5 W. The theory behind laser therapy is that chromophores (molecules in melanin and hemoglobin) absorb specific wavelengths of energy that are emitted by a laser, and this absorbed energy helps to activate enzymes and promote chemical reactions needed for cell function and tissue healing.
What is it used for?
Laser therapy can be used to treat a range of conditions due to its ability to reduce pain and inflammation and promote tissue healing. Hot lasers also produce thermal effects such as vasodilation and enhanced tissue repair.
Parameters:
Lower wavelength and frequency light penetrate tissue more deeply. Therefore, lasers with a wavelength between 600-1300 nm are typically used in physiotherapy treatment. More specifically, common types of lasers are red waveband (600-700 nm) and infrared waveband (700-950 nm) lasers.
There is more than one method to calculate treatment dose and time and there is a debate in the literature over which one to use. One method is as follows.
1. Determine the power density (W/cm) of your laser: Power density (W/cm) = average power (W) / beam spot size (cm)
2. Choose an appropriate dose (energy density, J/cm) that you wish to deliver to the tissues based on practice guidelines or manufacturers' instructions.
3. Calculate the time required to deliver this dose to one treatment point, considering the energy density of your laser: Treatment time (seconds) = energy density (J/cm) / power density (W/cm)
Note: Joules = Watts * seconds. Therefore, the units in the equation cancel out, leaving seconds as the unit for treatment time.
When providing laser therapy, ensure that you and your patient wear goggles that are made for the wavelength of your laser, to prevent injury to the eyes.
Contraindications:
Do not employ laser therapy over the eyes, abdomen during pregnancy, a malignancy (avoid moles), acute hemorrhage, thrombosis/phlebitis, cervical autonomic plexus or an implanted pacing device. Do not provide laser therapy to a patient with hypersensitivity to light or epilepsy/seizure disorder, who is taking immunosuppressants, or who has impaired sensation or cognitive impairments that may make it difficult for them to understand or communicate if they are experiencing discomfort.
Conclusion
The key to using EPAs effectively is understanding how they can be used as an adjunct to your broader plan of care. We hope this blog has been informative and helpful in reviewing commonly used EPAs and will help you understand when and how they can be employed to promote better outcomes for your patients. Good luck!
Thermal Agents |
|
HeatHeat tissues to ~ 45 degrees celsius. Specific parameters will depend on the kind of heating modality you are using, refer to the manufacturer’s instructions. |
ColdApply crushed ice over a damp towel for: 10 minutes to modulate pain 18-20 minutes to cool deeper tissues/prevent inflammation Specific parameters for other cold modalities will depend on the kind of modality being used, refer to the manufacturer’s instructions. |
Ultrasound |
|
Non-thermal ultrasoundMode: pulsed Duty cycle: 1:4 or 20% Intensity: 0.5-1 W/cm SATP or 0.1-0.2 W/cm SATA Frequency: 1 Hz for deep tissue, 3 Hz for superficial tissues Time: 10-15 minutes per 10 cm |
Thermal ultrasoundMode: continuous Intensity: 0.8-2 W/cm SATP, start at 0.8 until the patient feels heat and then do not increase further. Frequency: 1 Hz for deep tissue, 3 Hz for superficial tissues Time: 10-15 minutes per 10cm |
TENS |
|
C-TENSFrequency: 80-120 Hz Pulse duration: 150-200 µs Intensity: Increase slowly until the patient feels a sub-noxious tingling sensation Time: As long as necessary Electrode placement: Over the area of pain, bracketing the pain, over the dermatome, or over muscles at the corresponding spinal level |
A-TENSFrequency: 3-10 Hz Pulse duration: 250 µs Intensity: Increase slowly until a non-painful muscle twitching occurs. Time: 15-30 minutes, maybe repeated after 4 hours, as needed. Electrode placement: Over the dermatome, trigger points or acupuncture points |
IFC |
|
Acute pain relief IFCCarrier frequency: 4000 Hz AMF: 80-120 Hz Frequency sweep: Gradual 6 sec. up, gradual 6 sec. down Time: 20-30 minutes Electrode placement: Over the area of pain, bracketing the pain, over the dermatome, or over muscles at the corresponding spinal level. If using suction electrodes: Constant suction |
Longer-term pain relief IFCCarrier frequency: 4000 Hz AMF: 1-10 Hz Frequency sweep: Abrupt, 6 sec. high, gradual 6 sec. low Time: 20-30 minutes Electrode placement: Over the area of pain, bracketing the pain, over the dermatome, or over muscles at the corresponding spinal level. If using suction electrodes: Intermittent suction |
NMES |
||
StrengthWaveform: Symmetric biphasic Frequency: 50 Hz Pulse duration: 300 µs On: Off ratio: 10:50 seconds Ramp up/down: 2 seconds Amplitude: Slowly increase until muscle fully contracts Repetitions: 10-15 reps, less if muscle fatigued Location of electrodes: One electrode over the motor point or nerve supply to the relevant muscle, and the other electrode distally. |
EnduranceWaveform: Symmetric biphasic Frequency: 25-30 Hz Pulse duration: 300 µs On: Off ratio: 10:12 seconds, progress to 30:2 seconds Ramp up/down: 2 seconds Amplitude: Slowly increase until muscle fully contracts Time: 10-15 minutes, progress to hours Location of electrodes: One electrode over the motor point or nerve supply to the relevant muscle, and the other electrode distally. |
SpasticityFrequency: 35-50 Hz Pulse duration: 15-200 µs for small muscles or 200-350 µs for large muscles On: Off ratio: 2-5: 2-5 seconds, should be the same amount of time on vs off Ramp up/down: minimum 1 second Amplitude: Slowly increase until muscle fully contracts Time: 10-30 minutes, every 2-3 hours, until spasticity decreased. Location of electrodes: Apply one electrode to spastic muscle or its antagonist muscle, over the motor point or nerve supply to the relevant muscle, other electrodes distally. |
Iontophoresis |
||
|
Current type: Galvanic/direct Total dose: 40mA*min Safe current density: 0.1-0.3 mA/cm Amplitude (mA) = safe current density (mA/cm) x electrode area (cm) Treatment time (minutes) = total dose (mA*min) / amplitude (mA) Electrode placement: Place one electrode over the area of desired medication delivery, and the other electrode over a remote site. Note, the second electrode can be larger, to disperse the current. |
||
LASER |
||
|
Wavelength: 600-1300 nm, e.g. red waveband (600-700 nm), infrared waveband (700-950 nm) lasers Power density (W/cm) = average power (W) / beam spot size (cm) Dose i.e. energy density is measured in J/cm. Refer to practice guidelines or manufacturers' instructions. Treatment time per point (seconds) = energy density (J/cm) / power density (W/cm) |
||
Disclaimer: Embodia Inc and the authors of this document are not responsible for the application of the above modalities in patients, which should be performed appropriately and safely at the sole discretion and responsibility of the clinician.
References
Cotler, H. B., Chow, R. T., Hamblin, M. R., & Carroll, J. (2015). The Use of Low Level Laser Therapy (LLLT) For Musculoskeletal Pain. MOJ orthopedics & rheumatology, 2(5), 00068. https://doi.org/10.15406/mojor.2015.02.00068
ELECTROPHYSICAL AGENTS - Contraindications And Precautions: An Evidence-Based Approach To Clinical Decision Making In Physical Therapy. (2010). Physiotherapy Canada. Physiotherapie Canada, 62(5), 1–80. https://doi.org/10.3138/ptc.62.5
Gabison, S. (2019). Laser [PowerPoint slides]. Department of Physical Therapy, University of Toronto.
Gabison, S. (2019). Musculoskeletal Physiotherapy I: Electrophysical Agents (EPAs) Manual. Department of Physical Therapy, University of Toronto.
Gabison, S. (2020). Specialized Currents and Modalities, Unit 8 [PowerPoint slides]. Department of Physical Therapy, University of Toronto.
Goats G. C. (1990). Interferential current therapy. British journal of sports medicine, 24(2), 87–92. https://doi.org/10.1136/bjsm.24.2.87
Johnson M. (2007). Transcutaneous Electrical Nerve Stimulation: Mechanisms, Clinical Application and Evidence. Reviews in pain, 1(1), 7–11. https://doi.org/10.1177/204946370700100103
Rawat, S., Vengurlekar, S., Rakesh, B., Jain, S., & Srikarti, G. (2008). Transdermal delivery by iontophoresis. Indian journal of pharmaceutical sciences, 70(1), 5–10. https://doi.org/10.4103/0250-474X.40324
Takeda, K., Tanino, G., & Miyasaka, H. (2017). Review of devices used in neuromuscular electrical stimulation for stroke rehabilitation. Medical devices (Auckland, N.Z.), 10, 207–213. https://doi.org/10.2147/MDER.S123464
---
Blog writers: Bella Levi, MScPT student; Debra Posluns, MScPT student; Linnea Thacker, MScPT student
---
Date written: 30 Sep 2020
Last update: 17 Dec 2025
